Definition:
Wrong component transfused (WCT)
Where a patient was transfused with a blood component of an incorrect blood group, or which was intended for another patient and was incompatible with the recipient, which was intended for another recipient but happened to be compatible with the recipient, or which was other than that prescribed e.g. platelets instead of red cells.
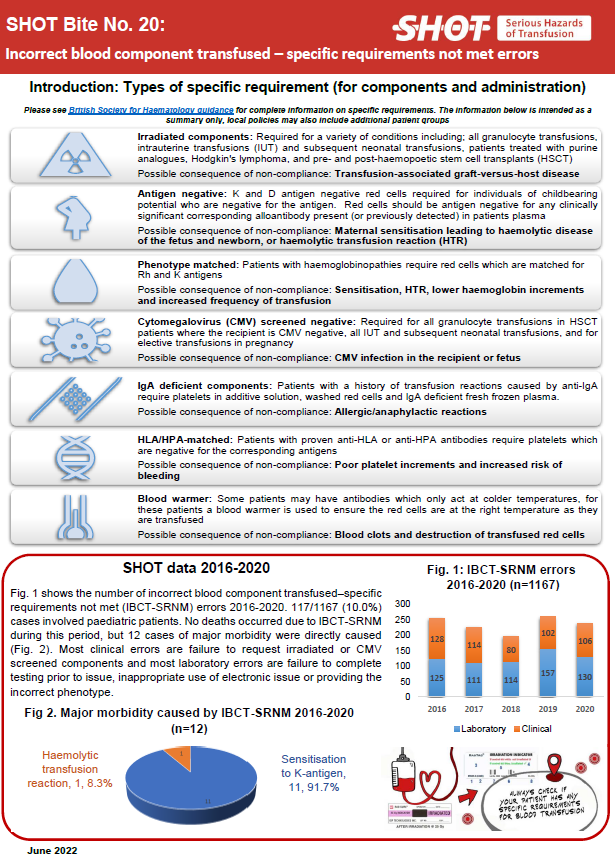
Specific requirements not met (SRNM)
Where a patient was transfused with a blood component that did not meet their specific requirements, for example irradiated components, human leucocyte antigen (HLA)-matched platelets when indicated, antigen-negative red cell units for a patient with known antibodies, red cells of extended phenotype for a patient with a specific clinical condition (e.g. haemoglobinopathy), or a component with a neonatal specification where indicated. (This does not include cases where a clinical decision was taken to knowingly transfuse components not meeting the specification in view of clinical urgency).
SHOT has collected data on incorrect blood component transfused (IBCT) since 1996. Originally, this category included all error reports, for example, avoidable transfusions, handling and storage errors, administration of anti-D immunoglobulin, and right blood to the right patient. In later years, these categories were separated out and reported in their own chapters.
The figure above only includes wrong component transfused (WCT) and specific requirements not met (SRNM) cases (plus some miscellaneous cases that did not fit easily into these categories. The remaining cases for Anti-D Ig, ADU, HSE and RBRP (where identifiable) have been included in the data drawers for those categories.
SHOT Transfusion Safety Standards
The SHOT Transfusion Safety Standards were released in July 2025, and these replace recommendations in the Annual SHOT Reports. More details on these can be found at: https://www.shotuk.org/transfusion-safety/transfusion-safety-standards/
Recommendations from recent Annual SHOT Reports (prior to 2024)
Accurate and complete patient identification (PID) is fundamental to transfusion safety. Training in correct PID procedures must be provided to all staff
Action: All staff in transfusion, ward managers
Transfusion competency training and assessment should be audited for effectiveness, particularly following errors. Competency-assessment should not just be a tick-box exercise
Access to specialist transfusion advice should be available to all transfusion staff at all times
Action: Transfusion laboratory managers, ward managers
Please see the individual SHOT chapters at the end of the page for other previous recommendations which remain relevant.
IBCT Resources
Please also see relevant videos on ABO-incompatible transfusions, pre-transfusion blood sampling and the pre-administration blood component transfusion bedside check. These can be accessed at the following link:
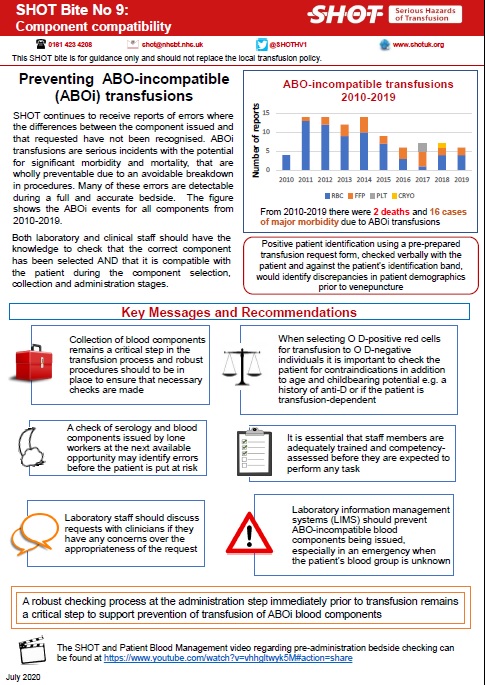
SHOT Bite No. 9: Component Compatibility
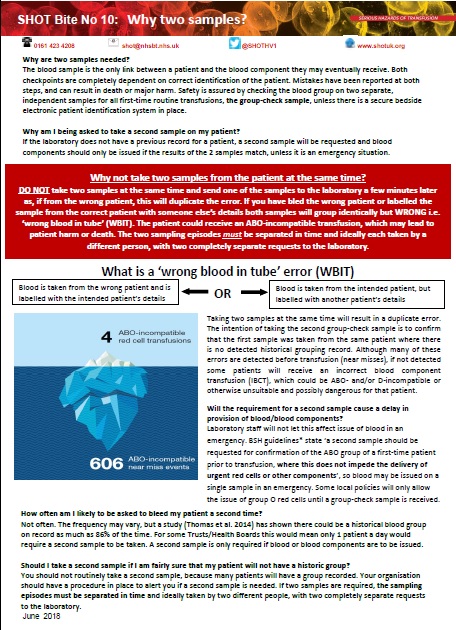
SHOT Bite No. 10: Why 2 Samples?
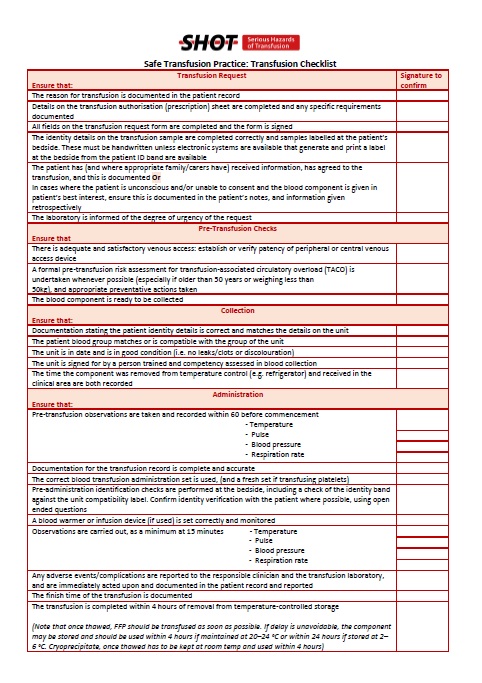
Safe Transfusion Practice – Transfusion Checklist
IBCT Annual Report Chapters
To access the chapter click either on the cover of the Annual SHOT Report or the link below the picture